Medical billing involves every step of the association between patients and healthcare providers. From the pre-registration process to the point of visit completion, the process consists of extracting patient data, verifying eligibility, checking medical billing codes, and approving healthcare insurance claims. However, for the most part, medical billing can be time-consuming for healthcare providers.
Automated medical billing is the way to ensure on-time reimbursement. Implementing automated medical billing software enables healthcare providers to generate medical bills and submit timely claims using AI and intelligent data extraction capabilities. AI in medical billing shortens the payment cycle and reduces operational billing costs. In this blog, we will explore how automated medical billing can reduce healthcare costs, expedite the reimbursement process, and improve cash flow.
Why Medical Billing Need Automation?
An automated medical billing system streamlines repetitive tasks like data entry, claims submission, and medical coding to speed up the reimbursement process. Below are some reasons medical billing automation is mandatory for healthcare providers.
- Lack of Proper Documentation
A recent report stated that 74% of healthcare providers use paper-based medical billing. On average, healthcare providers complete 20000 medical forms annually; each paper document filling costs $20. Given the extensive administrative work involved in medical billing, such as patient registration, eligibility checks, and claims validation, healthcare providers must prioritize proper documentation using automation solutions. - Incompatible Legacy Systems
Numerous healthcare providers still depend on outdated billing systems, necessitating staff to manually enter data. This results in substantial investments of time and finances as employees must process paper forms, input data into digital systems, and meticulously cross-check numbers to prevent errors. In a recent healthcare payment report, around 67% of consumers want digital and electronic payment options. In the face of mounting financial constraints and changing customer preferences, medical billing automation is a win-win for healthcare providers and patients. - Medical Coding Errors
A report estimated that 12% of healthcare insurance claims are submitted with the wrong medical coding. Medical coding involves translating procedures, surgeries, services, and treatments into standardized medical codes, providing hospitals with a shared billing language. However, the challenge arises when coders are presented with illegible handwritten notes from doctors or incomplete forms, halting the coding process.
What to Automate in Medical Billing Process?
- Patient Registration
A patient care journey starts with registration; automated medical billing software can simplify the registration process. Automation solutions enable medical billers to quickly extract and verify patient data from registration forms using intelligent data extraction and add it to the healthcare system. - Insurance Eligibility Check & Appointment
After patient registration, healthcare providers must check the patient coverage details to ensure bills are correctly assigned and prescriptions are covered for the bill’s entity. AI bots can easily capture patient insurance details from their ID cards and check insurance eligibility by logging into the insurance portal and scheduling appointments.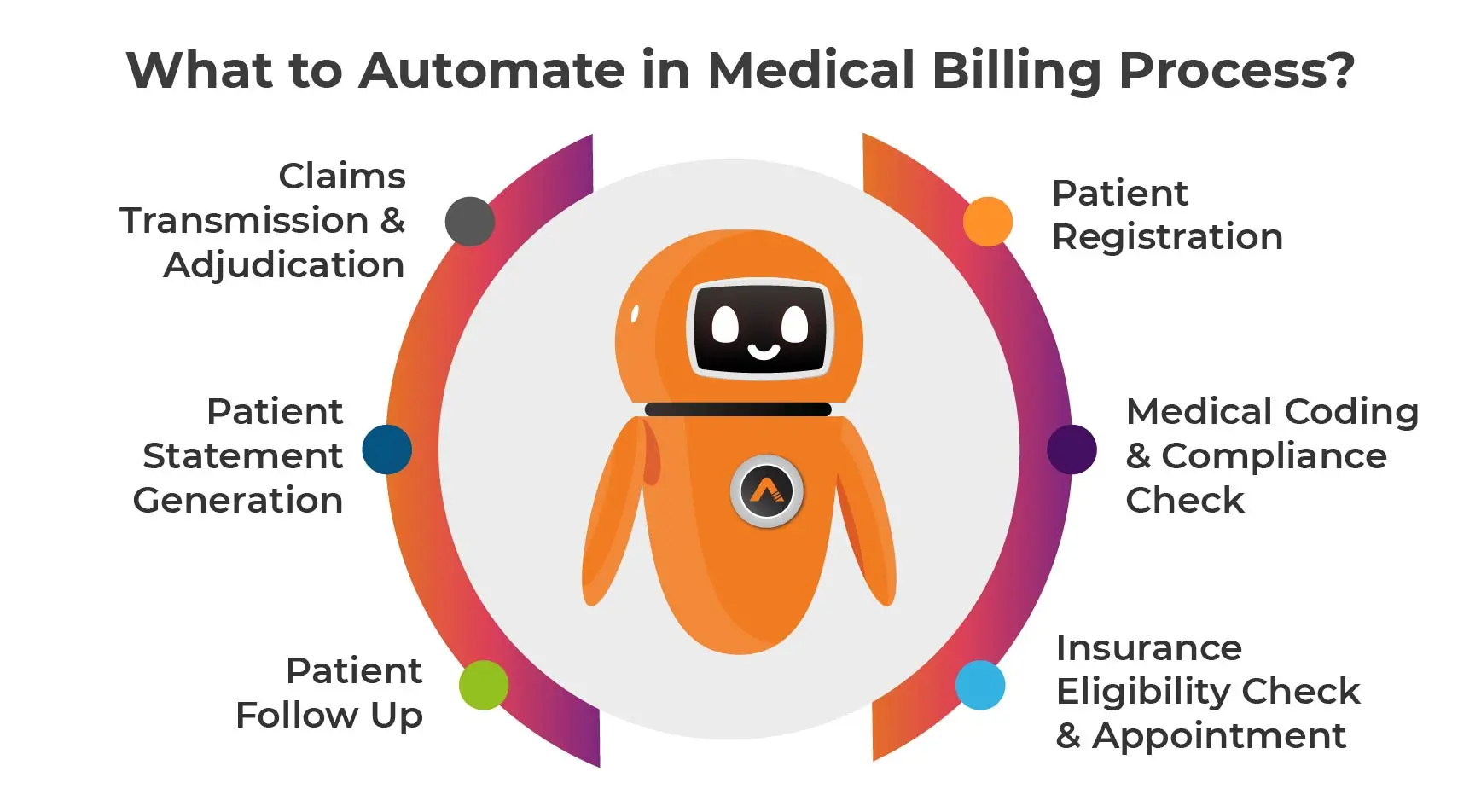
- Medical Coding & Compliance Check
Automation and advanced algorithms can analyze medical documents and assign appropriate medical codes for billing. Automated medical billing systems ensure that medical codes comply with HIPAA regulations. It also facilitates the generation of insurance claims by compiling all relevant information, including patient demographics, provider details, and procedural codes. Once the claims are compiled, they are electronically submitted to insurance companies, expediting the reimbursement process and reducing the administrative burden on healthcare providers. - Claims Transmission & Adjudication
As per HIPAA regulations, all healthcare providers must submit claims electronically. RPA in medical billing can be used to ensure claims are processed error-free. Besides claims transmission, an automated medical billing system provides an accurate claims adjudication process to inform patients whether a claim is accepted or rejected. Healthcare providers can quickly assess claims by comparing them against the pre-defined rules, policy terms, and historical data to evaluate coverage eligibility and determine payment amounts. - Patient Statement Generation
Automated patient statements comprehensively outline all services provided by the healthcare provider. These statements include the bill for procedures, with patients responsible for any remaining payments after the payer settles the agreed-upon amount. Additionally, specific payers may provide an Explanation of Benefits (EOB) to clarify the coverage details for procedures, including explanations for any discrepancies in coverage. Healthcare providers can share these statements automatically using email automation with their patients. - Patient Follow Up
Medical billing automation is vital in this process, as it can streamline bill generation, delivery, and payment reminders. Automated systems can schedule and send bills electronically, reducing the reliance on manual mailing processes. Additionally, they can send automated notifications to patients regarding upcoming payments or overdue balances. By implementing automation, healthcare providers can improve the efficiency of their billing operations and enhance their revenue cycle management.
Conclusion
As technologies continue to evolve, the capabilities of automated medical billing will only expand. Implementing medical billing automation can ensure interoperability between different healthcare IT systems, ensuring accurate medical billing and a better return on investment. AutomationEdge’s CareFlo ICD Coding bot enables healthcare providers to reduce manual effort in coding search and allow/reject updating the ICD codes identified by the AI system. Contact us to learn more about AutomationEdge CareFlo.
The post Automated Medical Billing for Faster Reimbursement appeared first on AutomationEdge.
This is a companion discussion topic for the original entry at https://automationedge.com/blogs/automated-medical-billing-for-faster-reimbursement/